In recent years, dermatology has witnessed a growing shift toward more precise, patient-friendly treatment solutions. Among these innovations,311 nm narrowband ultraviolet B (NB-UVB) phototherapyhas become increasingly recognized as a cornerstone therapy for a range of chronic inflammatory and pigment-related skin conditions. As clinical understanding deepens and device technology evolves, phototherapy is no longer confined to specialized hospital departments but is gradually extending into outpatient and home-care environments.
Ultraviolet light has long been used in dermatological treatment, yet not all UV wavelengths offer the same balance of efficacy and safety. The 311 nm wavelength represents a carefully selected segment of the UVB spectrum that maximizes therapeutic benefits while minimizing unnecessary skin exposure. Unlike broad-spectrum UV radiation, which includes wavelengths associated with erythema and long-term skin damage, narrowband UVB concentrates energy where it is most clinically useful.
At the epidermal level, 311 nm UVB interacts directly with keratinocytes, immune cells, and melanocytes. This targeted interaction explains why the wavelength has shown consistent success across multiple skin conditions with different pathological mechanisms.
Vitiligo is characterized by the progressive loss of melanocytes, resulting in depigmented patches that can significantly affect a patient’s appearance and psychological well-being. Clinical research indicates that NB-UVB phototherapy can stimulate remaining melanocytes and activate melanocyte stem cells located in hair follicles. Over time, these cells migrate into depigmented areas, supporting gradual repigmentation.
Compared to uncontrolled sun exposure, 311 nm phototherapy provides reproducible dosing and predictable outcomes. This consistency is especially important for vitiligo patients, whose treatment success depends on long-term adherence and precise exposure management.
Psoriasis is driven by immune dysregulation that accelerates skin cell turnover, leading to thickened, inflamed plaques. NB-UVB therapy plays a critical role by slowing keratinocyte proliferation and modulating inflammatory pathways. By influencing cytokine production and T-cell activity within the skin, phototherapy addresses both the visible symptoms and the underlying immune imbalance.
In addition to psoriasis, conditions such as eczema and pityriasis rosea often involve chronic inflammation and impaired skin barrier function. Controlled UVB exposure has been shown to reduce itching, calm inflammation, and support skin recovery when used under appropriate protocols.
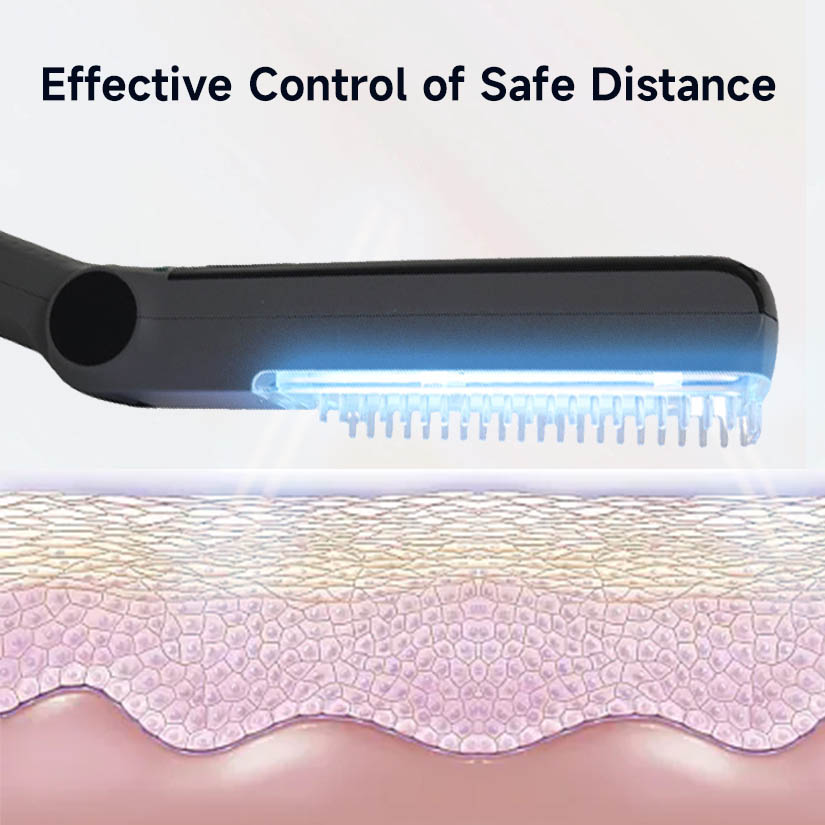
The effectiveness of phototherapy depends not only on wavelength selection but also on how uniformly and accurately light is delivered to affected skin. Modern UVB phototherapy systems are designed to provide even energy distribution across the treatment area, reducing hotspots and minimizing the risk of overexposure.
By focusing light precisely where it is needed, clinicians and patients can achieve meaningful results with lower cumulative doses. This approach aligns with the broader medical trend toward precision therapy—treatments that are tailored, controlled, and evidence-based.